I’ve chosen again to put together a digest of what’s happening related to COVID-19 the past few days. Each item is denoted with a bullet and I’ve bolded the state or title that applies to the material you’ll want to check out.
- The state of New Jersey, Department of Health, issued Executive Directive No. 20-026 on August 10, 2020. This is a 41-page document is also entitled: Directive for the Resumption of Services in all Long-Term Care Facilities.
The Directive affects long-term care facilities, assisted living residences, comprehensive personal care homes, residential healthcare facilities and dementia care homes. This reopening plan is comprised of four phases, which are tied to the state’s planned stages for reopening. All NJ facilities started in Phase 0 on August 10th.
These LTCFs must comply with the following in order to enter the next reopening phase:
- Contract with an infection control service within two months or hire a full-time infection control employee if they have more than 100 beds or hemodialysis;
- Develop an updated outbreak plan with lessons learned from the COVID-19 pandemic. This plan must include a communications strategy that outlines regular communication with residents and families about cases and outbreaks or any other emergency and methods for virtual communication in the event of visitation restrictions;
- Implement a respiratory protection program that complies with OSHA standards, including medical screenings and fit testing of employees using respirators (N95 masks), within nine months;
- Must be fully staffed and have a plan in place for additional staffing in the event of an outbreak or emergency;
- Weekly COVID-19 testing of staff until guidance from the NJDOH changes based on epidemiology and data about the circulation of virus in the community;
- Secure enough personal protective equipment (PPE) for present use and a stockpile for emergencies;
- Must not have an active outbreak.
The state of New Jersey announced that it is making $155 million available to help these facilities safely reopen with about $25 million to assist with the weekly testing. New state Medicaid funding of $130 million will be available beginning in October and running through June 30, 2021. Of that, $52 million is intended to help LTCFs in supporting COVID-19-related infection control and compliance. However, the funding would be subject to recoupment if a facility fails to meet the DOH-specified requirements or is found to have repeated infection control failures. The remaining $78 million will go toward increasing wages for certified nurse aides.
There is a lot of guidance within this document so please review it carefully and keep it handy for reference. You’ll appreciate the colorful charts found on the last 6 pages of the Directive.
- COVID-19 in LTC Office Hours: Join Our Discussion About COVID-19 Required Data with State Health Department’s HAI Experts
Thursday, September 3, 2020
1pm MT | 2pm CT | 3pm ET
Nursing homes are on the front-line in the fight against COVID-19. In the mist of the challenges that come with being on the front-line, nursing homes are facing the necessity of public health reporting while working to implement prevention and preparedness guidance. Do you have questions and uncertainty? Join us for an “Office Hours” session for nursing home providers with the Telligen Nursing Home Team. This interactive session will provide nursing home personnel and infection preventionists with the opportunity to get answers directly from infection prevention public health experts in Colorado, Illinois, Iowa and Oklahoma as well as resources for implementing current CDC guidance. Attendees will also have an opportunity to share their approaches and learn from one another.
Please join us for a conversation with Healthcare Associated Infection (HAI) experts from Colorado, Iowa, Illinois, and Oklahoma’s public health departments. Participants will have the opportunity to ask questions and interact with the HAI division representatives. The experts will share information about the critical value of surveillance reporting and how the data is used.
- Assisting Nursing Homes to Remain Prepared During the Ongoing COVID-19 Public Health Emergency
Wednesday, September 9, 2020
11am MT | 12pm CT | 1pm ET
Join us for an upcoming webinar focused on Assisting Nursing Homes to Remain Prepared During the Ongoing COVID-19 Public Health Emergency. You will learn about approaches that nursing homes can take to better prepare for COVID-19 surges. Speakers will also review the CMS hot spot strategy, which directs additional resources to nursing homes in COVID-19 hot spot areas, and define what hot spots are. Be on the lookout for additional details in the coming weeks. Registration is required.
- The Texas Health and Human Services Commission has published guidelines for long-term care facilities to follow to allow for Phase 1 visitation. These guidelines pertain to nursing facilities, assisted living facilities and intermediate care facilities for individuals with an intellectual disability or related conditions. Read this document to understand the requirements.
- Does Universal Testing for COVID-19 Work for Everyone? This is a pre-proof of an article accepted August 13, 2020 for publication in the Journal of the American Medical Directors Association. The Brief Summary provided in the pre-proof notes that “Universal testing for SARS-CoV-2 is only one part of broader infection prevention and control efforts nursing homes must take to reduce the risk of residents developing COVID-19 infections.”
The authors review “the tests available to diagnose COVID-19 infections, the implications of universal testing for nursing home staff and residents, interpretation of test results, issues around repeat testing, and incorporation of test results as part of a long-term response to the COVID-19 pandemic and propose a structured approach for facility-wide testing of resident and staff and provide alternatives if testing capacity is limited, emphasizing contact tracing. Nursing homes with strong screening protocols for residents and staff, that engage in contact tracing for new cases, and that continue to remain vigilant about infection prevent and control practices, may better serve their residents and staff by thoughtful use of symptom- and risk-based testing strategies.”
The case study is interesting – involves a 134-bed nursing home in northeast Georgia. The authors speak to various events that occur with the introduction of coronavirus into the facility and how the infection is managed. Questions are posed and answered in the abstract. Implications for practice and policy are discussed. This is the authors conclusion:
“Universal testing may have a role in helping to guide nursing homes’ responses to the COVID-19 pandemic. Testing, however, is only one of many measures needed to prevent the spread of SARS-CoV-2 among the frail elders living in congregate settings. Nursing homes with strong screening protocols for residents and staff, that engage in contact tracing for new cases, and that continue to remain vigilant about infection prevent and control practices, may better serve their residents and staff by thoughtful use of symptom- and risk-based testing strategies.”
Very useful information is also provided, starting on page 25 of the 32-page pre-proof including:
- Enhanced Screening Criteria for COVID-19 Infection in Nursing Home Residents
- Overview of Tests for SARS-CoV-2 (includes CPT codes and approximate costs)
- Preparedness Checklist for Facility Wide Testing
- Numerous references
This is a good read!
- Interim Guidance for Rapid Antigen Testing for SARS-CoV-2 was updated August 16, 2020.
- Guidance for General Laboratory Safety Practices during the COVID-19 Pandemic was updated August 15, 2020. This guidance is to address the general workflow safety concerns of laboratory personnel during the COVID-19 pandemic. All laboratories should perform site- and activity-specific risk assessments to determine the most appropriate safety measures to implement for particular circumstances. In addition, facilities should adhere to local policies and procedures as well as all applicable federal, state, and local regulations and public health guidelines.
- MLN Matters Number: SE20015 was revised August 17, 2020. The title of this article is: New COVID-19 Policies for Inpatient Prospective Payment System (IPPS) Hospitals, Long-Term Care Hospitals (LTCHs), and Inpatient Rehabilitation Facilities (IRFs) due to Provisions of the CARES Act.
The revised information is found on pages 2 and 3 of the article. The revisions start with:
Keep reading the MLN Matters to see all of the revised information regarding billing.
- Communication with Patients and Families Regarding Health Care–Associated Exposure to Coronavirus 2019: A Checklist to Facilitate Disclosurewas published June 3, 2020 in The Joint Commission Journal on Quality and Patient Safety. This is a commentary worth reading. You can read it online or download in PDF (icon in upper right corner of the webpage).
“As the novel coronavirus 2019 (COVID-19) pandemic unfolds, health care institutions will need to grapple with the challenge of notifying patients and their family members about possible or known exposures to the virus. This task will become increasingly monumental as the virus rapidly multiplies within communities. It will be critical for health care organizations to use a standardized, robust, and clear communication strategy to notify and guide patients in the ambulatory setting. Each organization will need to identify a disclosure team with the capacity to respond rapidly to clinical questions about symptoms and prognosis; to instruct patients on containment strategies; to provide supportive responses to emotional distress; to help patients and their families connect with resources they need in order to adhere to recommendations such as wearing masks, self-quarantine, and diagnostic testing; and to systematically track and notify at-risk patients and those proximally associated with them.
We have developed a pragmatic COVID-19 exposure disclosure checklist (Table 1) to standardize the disclosure process and ensure that all key areas are considered in every conversation. There are five core competencies that are critical to facilitating an effective COVID-19 exposure disclosure conversation: clinical, infectious disease, risk management, language, and psychosocial (Table 2). Skill in cultural sensitivity, clear communication, and emotional intelligence is also helpful.”
- QSO-20-36-ESRD … Key Components for Continued COVID-19 Management for Dialysis Facilitieswas issued August 17, 2020.
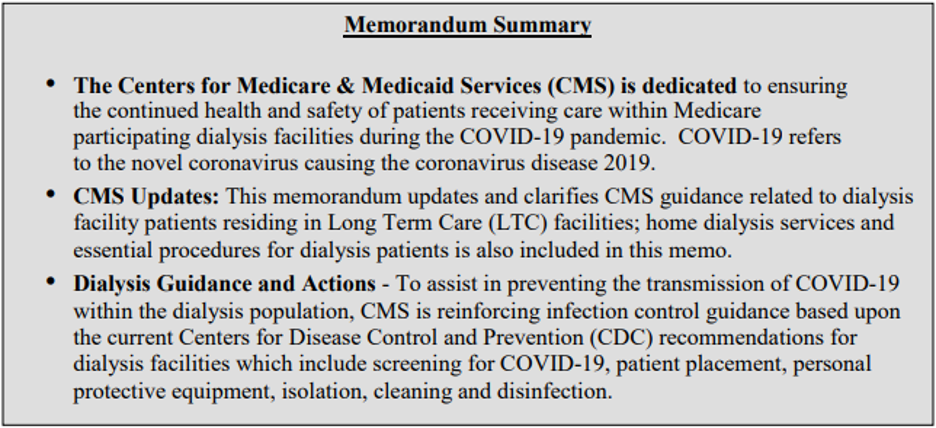
Note the second bullet above – this applies to dialysis facility patients residing in LTC facilities (page 3) as well as home dialysis.
A 5-page Checklist for Dialysis Facilities in COVID-19 Hotspots is also found with the posting of this QSO. This also speaks to LTC facilities with dialysis patients and home care.
Want to keep up with the changing COVID-19 situation in skilled nursing?