Optimal MDS 3.0 reimbursement requires a clear view
It’s no secret that analyzing and understanding data has become fundamental to success in any industry. In order to stay ahead of competition and changing regulations, businesses must not only have access to all their data, but be able to view it in an understandable and actionable way.
The key words here are understandable and actionable.
This is one reason we hear so much about dashboards these days. A dashboard provides a simple view of data and key performance indicators (KPIs) that relate to a particular business objective or process. The goal is to highlight key information about the business so that managers know where changes need to be made.
A limited view of MDS transmission data
A big reason that long-term care facilities fail to achieve optimal MDS 3.0 reimbursement, however, is that they don’t have a complete picture of their MDS 3.0 workflow.
Rather than seeing a top-level view of all MDS activity, which ideally includes an end-to-end picture of the workflow down to the individual MDS assessment and resident, MDS staff are often limited to manually searching on a granular basis for MDS rejects and exceptions. Because they don’t have the power to see the big picture, it’s easy to overlook errors and miss billing opportunities.
In addition, the limitations of accessing reports and data directly from CMS lead to easily missing key indicators. The data may be available from CMS, but is often overlooked because of the difficulty in accessing it.
How is reimbursement affected?
A limited view of MDS workflow can negatively affect MDS 3.0 reimbursement because it leads to:
- Missed billing opportunities. A limited view of data means that key indicators and billing opportunities are easily overlooked. Over time, this can add up to a big impact on an organization’s overall reimbursement.
- Compounding of errors over time. The manual process of MDS transmission, coupled with a lack of insight into the data, means that errors in transmission and data analysis more easily occur. This scenario only gets worse as the volume of data grows.
- Underperforming facilities. Without a top-level view of the MDS transmission workflow across multiple facilities, it’s impossible to compare performance of individual facilities and staff members. Both accountability and reimbursement can suffer.
The solution: A comprehensive MDS dashboard view
Trying to understand MDS workflow via a single manual transmission episode is like going through your day with a blindfold on. You can accomplish a few things are visible, but it’s far from the most efficient way to work.
To truly optimize MDS 3.0 reimbursement and minimize MDS errors, skilled nursing facilities need a full 360-degree view of their entire MDS process.
What would this kind of view look like? Here’s what SimpleMDS users are able to accomplish:
Simple dashboard view
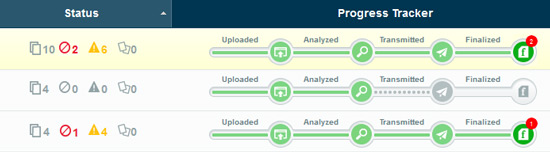
A 360-degree view of the MDS transmission process includes an intuitive dashboard view of all your MDS activity, allowing you instantly to see whether assessments were accepted, accepted with warnings or rejected. Staff can then instantly analyze problem areas and correct errors within minutes.
Sort and analyze MDS data
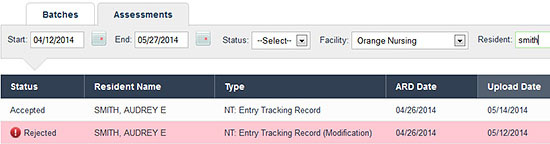
To quickly research rejected assessments, simply filter the assessment view to see only rejects. Your most recent assessment appears first and one click opens the Final Validation report to the error message. Another click and you can view the MDS as a PDF or in its native XML format and quickly assess the issue.
CMS reports at your fingertips
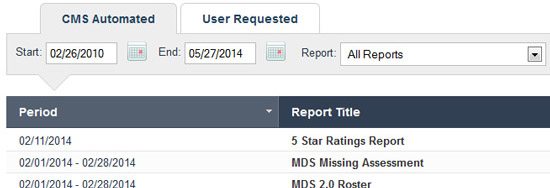
In addition, all your CMS and CASPER reports are accessible in one place. You can view and print Initial Feedback and Final Validation reports, as well as two years of MDS assessments, Initial Feedback and Final Validation reports. Items over two years old are automatically archived for retrieval at any time.
The takeaway
To truly optimize long-term care MDS 3.0 reimbursement and minimize MDS errors, facilities need to take off the blindfolds and see a full 360-degree view of their MDS processes. Is it time to evaluate whether your facility should automate MDS transmission?



