CORE Analytics: Compliance
Ensure your SNF claims fully comply with CMS rules and regulations
Identify potential risk areas and devise auditing strategies to ensure claims compliance and reimbursement success.
When it comes to third-party CMS audits, the claim files tell the story. In fact, all data-driven CMS audits are triggered by the claim files — and not the MDS (in most cases, auditing agencies don’t have access to MDS data, they only have the claims).
The challenge is that industry reports informing providers on potential risk areas are too old to devise auditing strategies around. Introducing our Statistical Analysis of Likely Targets (SALT) Report — a more current approach than waiting for the industry’s old PEPPER.
![]()
“Reimbursement” and “Compliance” are two sides of the same coin. CORE employs a data-driven approach to reimbursement compliance using current claims to help providers devise auditing strategies in compliance with CMS rules and regulations.
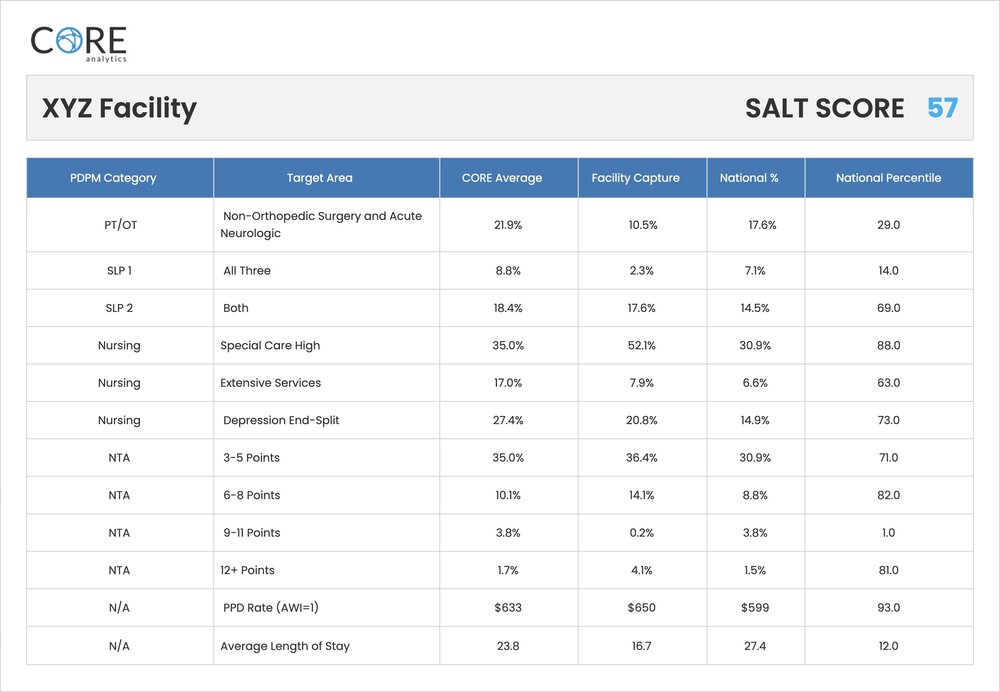
Identify outlier capture
Our SALT Report compares current facility capture in the “at-risk” PDPM target areas relative to the national average. We rank each facility within a national percentile, then weight each target area based on a proprietary algorithm developed by the nation’s leading SNF compliance auditing firm to produce a SALT score.
The weights of each target area are adjusted based on current auditing activity in the market. Providers use the data to direct both their internal and external (third-party) compliance auditing strategy mandated by CMS. You no longer need to wait for the PEPPER — which is based on old data and will not keep up with the case-mix creep (rapid evolution of PDPM categories in the new system).
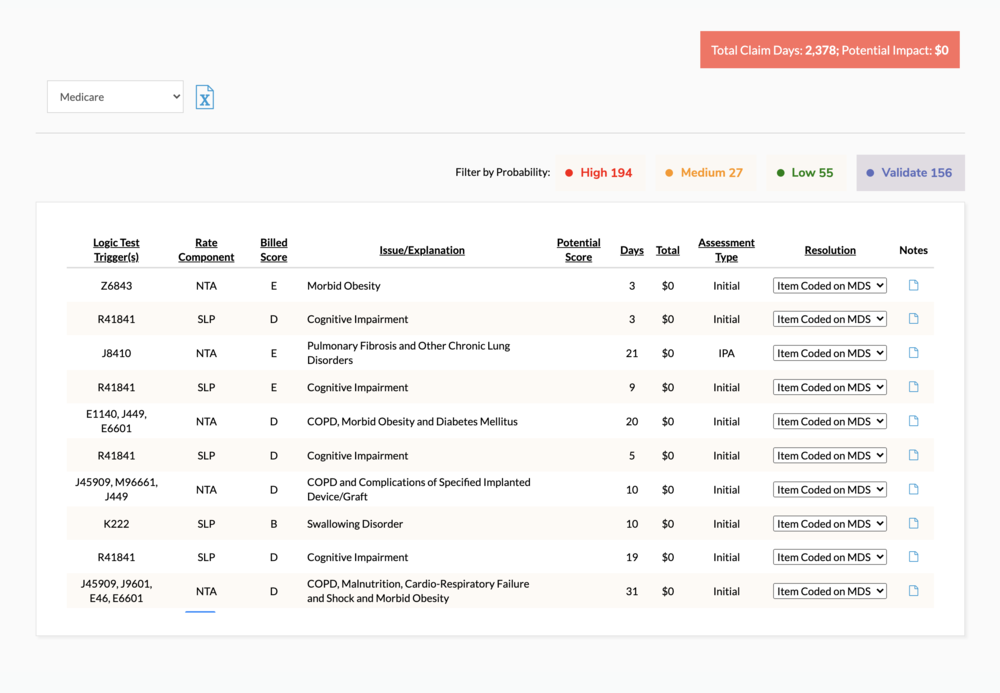
Strengthen claim coding
CORE logic tests point out inconsistencies between the billed score and various claim elements. The goal is to strengthen the accuracy of both the MDS score captured, and the various claim elements that are submitted to the MAC for payment.
The review provides the user with the opportunity to validate the accuracy of codes submitted on the claim file and ensure appropriate coding of the highest captured scores. Claim integrity is the foundation to a facility’s corporate compliance plan and data collection efforts for both fee-for-service Medicare, Managed Care and future payment iterations.
Get your free CORE demo
Book a personalized online demo to learn how CORE can help you identify opportunities for growth
Schedule demo




